Sarcoidosis, a systemic inflammatory disease characterized by the formation of non-caseating granulomas, typically affects the lungs and lymphatic system. However, its presentation can be quite varied, making diagnosis a challenge. Isolated splenic sarcoidosis, where the spleen is the primary or only affected organ, is a rare entity. This case highlights the importance of considering less common diagnoses when evaluating patients with unexplained splenomegaly, and underscores the role of thorough investigation, including biopsy, in reaching an accurate diagnosis.
The diagnostic journey often involves excluding more common causes first. In this particular instance, the clinicians acted as detectives, piecing together clinical clues, lab results, and imaging findings to finally arrive at the correct conclusion. It's a reminder that in medicine, the unusual can and does occur, demanding vigilance and a systematic approach.
Clinical Key Takeaways
lightbulb
- The PivotIsolated splenic sarcoidosis requires a high index of suspicion, particularly when common causes of splenomegaly have been ruled out. Consider it even without typical systemic symptoms.
- The DataA case report highlighted a patient presenting solely with splenomegaly, ultimately diagnosed with splenic sarcoidosis via biopsy, showcasing the necessity of invasive procedures in ambiguous cases.
- The ActionWhen faced with unexplained splenomegaly, proceed with a systematic workup, and strongly consider splenic biopsy if initial investigations are unrevealing, guiding subsequent management.
The Clinical Presentation
The patient's journey often begins with vague, non-specific symptoms, or, as in cases of isolated splenic sarcoidosis, with the incidental finding of splenomegaly on imaging. Unlike typical sarcoidosis, where pulmonary symptoms dominate, isolated splenic involvement can present without the classic cough, dyspnea, or chest pain. Instead, patients might report fatigue, abdominal discomfort, or early satiety due to the enlarged spleen pressing on other organs. Some individuals may even be asymptomatic, with the splenomegaly discovered during a routine physical exam or imaging study performed for an unrelated reason. This variability in presentation underscores the diagnostic challenge.
Diagnostic Workup and Challenges
When splenomegaly is detected, a systematic diagnostic approach is essential. Initial investigations typically include a complete blood count (CBC) to assess for cytopenias, liver function tests (LFTs) to evaluate liver involvement, and a peripheral blood smear to rule out hematologic malignancies. Serologic testing for infectious diseases, such as viral hepatitis and mononucleosis, is also crucial. Imaging studies, including ultrasound, CT scan, or MRI of the abdomen, can help characterize the spleen's size and appearance, and identify any associated lymphadenopathy or other organ involvement. However, these initial tests are often non-specific and may not provide a definitive diagnosis.
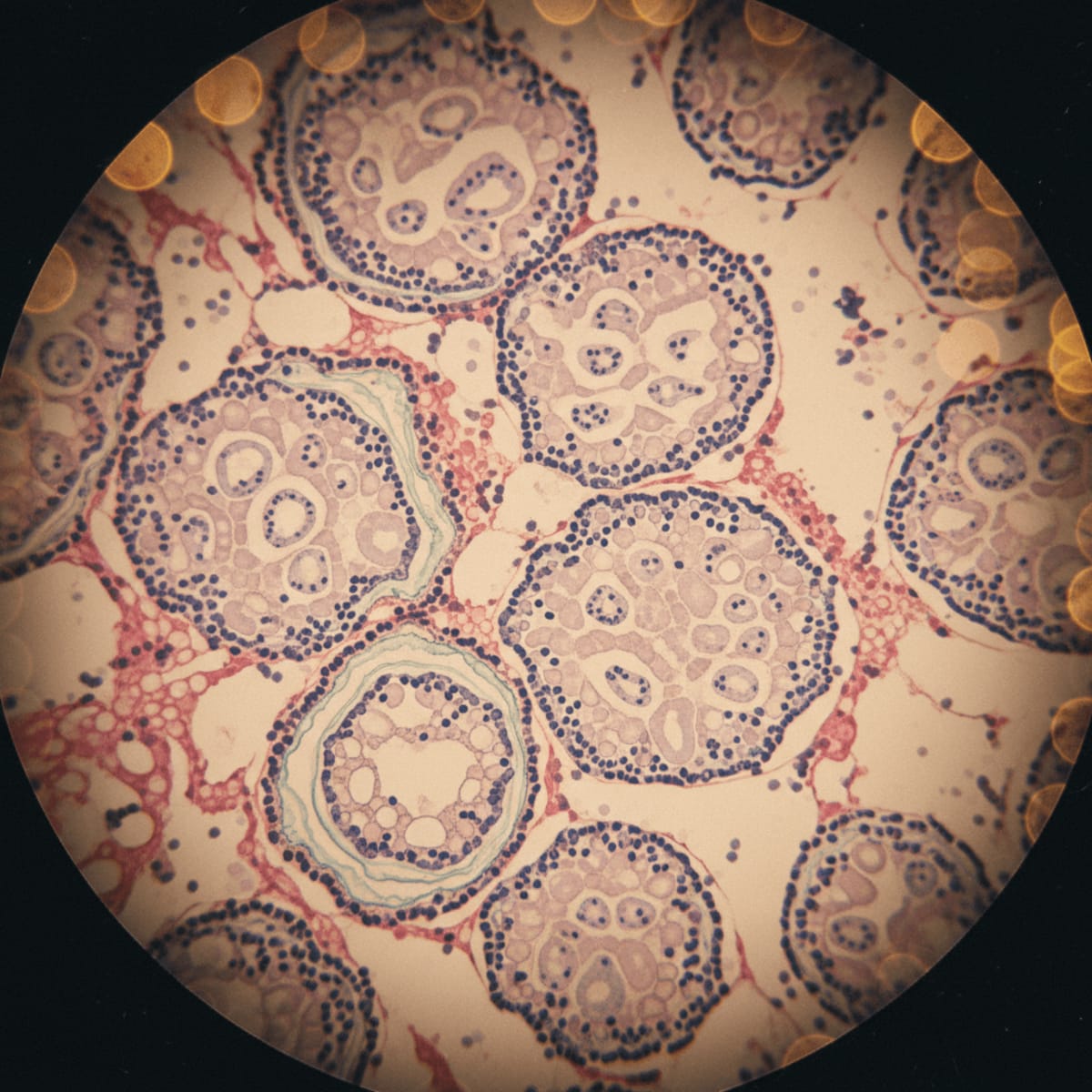
The real challenge lies in differentiating splenic sarcoidosis from other more common causes of splenomegaly, such as infections, hematologic malignancies, and liver disease. Lymphoma and leukemia, for instance, can both present with splenomegaly and systemic symptoms, mimicking sarcoidosis. Similarly, chronic liver diseases, such as cirrhosis, can lead to portal hypertension and subsequent splenic enlargement. In cases where the diagnosis remains uncertain despite initial investigations, a biopsy of the spleen is often necessary. This can be performed percutaneously or surgically, depending on the clinical circumstances and the availability of expertise. The biopsy sample is then examined under a microscope to look for the characteristic non-caseating granulomas of sarcoidosis. It is crucial to rule out other granulomatous diseases, such as tuberculosis or fungal infections, with appropriate staining and cultures.
Comparison to Existing Guidelines
While there are no specific guidelines that address isolated splenic sarcoidosis, the European Respiratory Society (ERS) guidelines on sarcoidosis provide a framework for diagnosing and managing the disease in general. These guidelines emphasize the importance of a multidisciplinary approach, involving pulmonologists, radiologists, and pathologists, among others. The ERS guidelines recommend considering sarcoidosis in patients with unexplained respiratory symptoms, lymphadenopathy, or organ involvement, and advocate for biopsy confirmation whenever possible. However, they do not specifically address the challenges of diagnosing isolated splenic involvement, which can be particularly difficult due to the lack of typical pulmonary findings. This highlights a gap in the existing guidelines and underscores the need for increased awareness of this rare presentation.
Limitations of Case Reports
Case reports, while valuable for highlighting unusual presentations and diagnostic challenges, have inherent limitations. They describe the experience of a single patient and may not be generalizable to other individuals with the same condition. Case reports are also subject to publication bias, meaning that reports of successful diagnoses or treatments are more likely to be published than those with negative or inconclusive results. Furthermore, case reports do not provide statistical evidence of the effectiveness of a particular diagnostic or therapeutic approach. In the context of isolated splenic sarcoidosis, case reports can help raise awareness of this rare entity, but they cannot replace larger, controlled studies that are needed to establish optimal diagnostic and management strategies. We also have to acknowledge the possibility of recall bias impacting clinical history reported in such reports.
Clinical Implications
The diagnostic odyssey for isolated splenic sarcoidosis can be resource-intensive, involving multiple imaging studies, laboratory tests, and potentially an invasive biopsy. This translates to increased healthcare costs and potential delays in diagnosis and treatment. Furthermore, the lack of specific diagnostic codes for isolated splenic sarcoidosis can complicate billing and reimbursement. Clinicians need to be aware of these challenges and advocate for appropriate coverage for patients with this rare condition. Workflow bottlenecks can arise if splenic biopsies require specialized expertise or equipment that is not readily available in all hospitals, potentially delaying diagnosis. A clear, evidence-based algorithm for investigating splenomegaly is needed to reduce the burden on both patients and healthcare systems.
Given the rarity of isolated splenic sarcoidosis, many pathologists may not immediately consider it in the differential diagnosis, potentially leading to diagnostic delays. Open communication between the clinician and the pathologist is crucial to ensure appropriate staining and evaluation of the biopsy specimen. Clinicians should also be aware of the potential for false-negative biopsies, particularly if the granulomas are sparsely distributed or if the biopsy sample is not representative of the entire spleen. In such cases, repeat biopsy or alternative diagnostic approaches may be necessary. The financial toxicity associated with extensive diagnostic testing should also be considered, and efforts should be made to streamline the workup and minimize unnecessary procedures.
LSF-9100883067 | December 2025

How to cite this article
Webb M. Uncommon presentation: the diagnostic challenges of splenic sarcoidosis. The Life Science Feed. Published January 20, 2026. Updated January 20, 2026. Accessed January 31, 2026. .
Copyright and license
© 2026 The Life Science Feed. All rights reserved. Unless otherwise indicated, all content is the property of The Life Science Feed and may not be reproduced, distributed, or transmitted in any form or by any means without prior written permission.
Fact-Checking & AI Transparency
This summary was generated using advanced AI technology and reviewed by our editorial team for accuracy and clinical relevance.
References
- Statement on sarcoidosis. American Thoracic Society, European Respiratory Society, World Association of Sarcoidosis and Other Granulomatous Disorders. Am J Respir Crit Care Med. 1999;160(2):736-755.
- Hunninghake, G. W., Costabel, U., Ando, M., Baughman, R., Cordier, J. F., du Bois, R., ... & Crystal, R. G. (1999). ATS/ERS/WASOG statement on sarcoidosis. American Thoracic Society/European Respiratory Society/World Association of Sarcoidosis and other Granulomatous Disorders. European Respiratory Journal, 14(4), 735-748.
- James, W. E., & Sharma, O. P. (2016). Splenic sarcoidosis: a review. Journal of Clinical Pathology, 69(1), 18-24.
- Newman, L. S., Rose, C. S., & Maier, L. A. (1997). Sarcoidosis. New England Journal of Medicine, 336(17), 1224-1234.