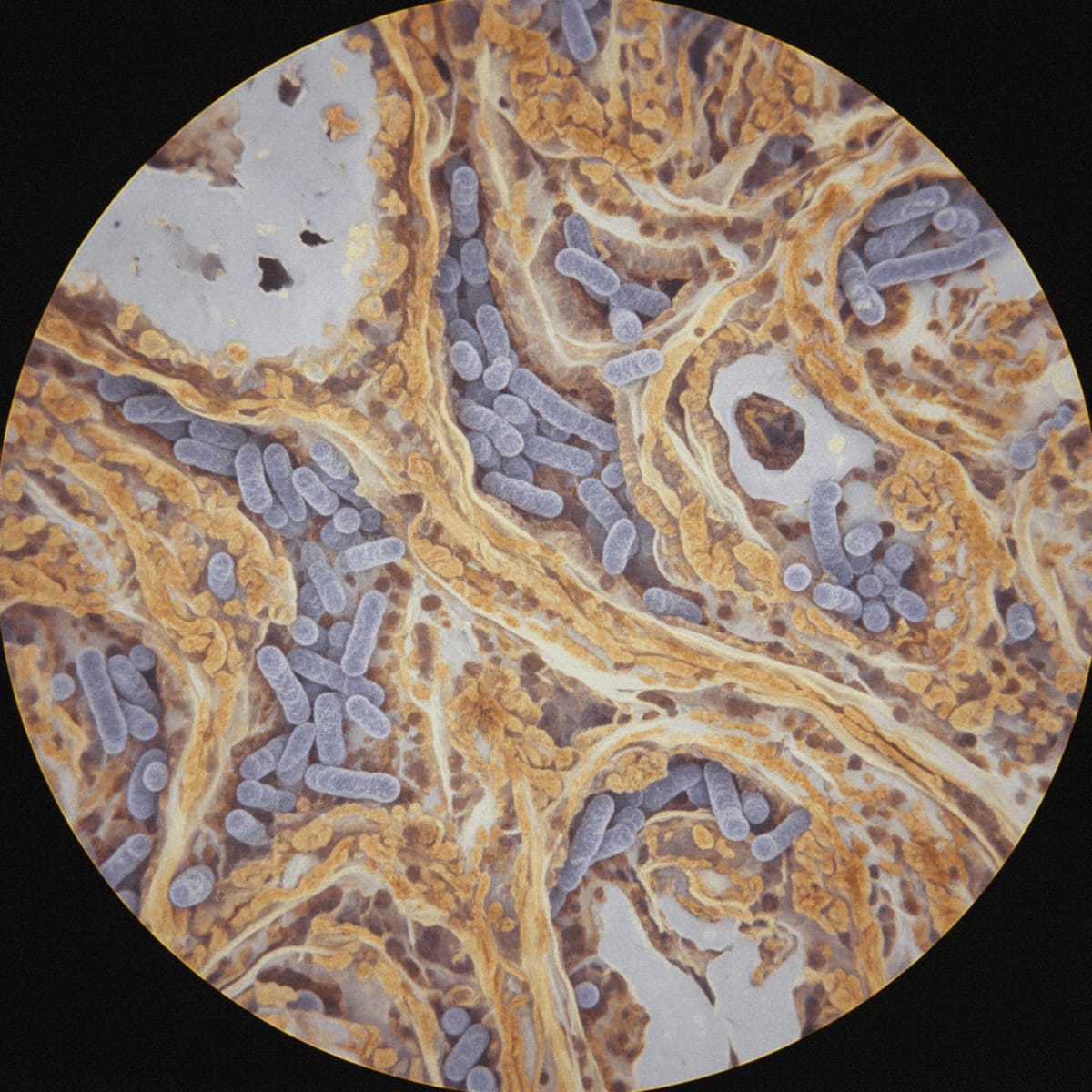
The intersection of rheumatologic disease and infectious complications presents a growing challenge. As we deploy increasingly potent immunosuppressive therapies for conditions like systemic sclerosis (SSc), the risk of opportunistic infections rises commensurately. This is particularly concerning in regions with a high prevalence of diseases like tuberculosis (TB). A recent case report serves as a stark reminder of this reality, highlighting the diagnostic and therapeutic complexities when pulmonary TB complicates SSc-associated interstitial lung disease (ILD).
While this is a single case, it forces us to re-evaluate our screening protocols and treatment strategies for patients with SSc, especially those residing in or originating from TB-endemic areas. Are our current guidelines sufficient, or do we need more proactive and targeted approaches to mitigate this risk?
Clinical Key Takeaways
lightbulb
- The PivotTB screening in SSc patients, particularly those with ILD in TB-endemic regions, needs re-evaluation for earlier detection. Current guidelines may be insufficient.
- The DataDelayed TB diagnosis can occur due to overlapping symptoms with ILD, leading to increased morbidity and mortality in SSc patients.
- The ActionImplement routine, high-sensitivity TB screening (e.g., interferon-gamma release assays) in SSc patients with ILD in high-risk regions, irrespective of reported TB exposure history.
The Diagnostic Challenge
Diagnosing pulmonary TB in patients with SSc-associated ILD presents a formidable challenge. Symptoms such as cough, shortness of breath, and fatigue are common to both conditions, masking the presence of TB until it reaches an advanced stage. Further complicating matters, the immunosuppressive medications used to manage SSc can blunt the typical inflammatory response to TB, leading to atypical radiographic presentations and delayed diagnosis. Are we, as clinicians, adequately equipped to differentiate between disease progression and opportunistic infection in this context?
The insidious nature of TB in immunosuppressed individuals necessitates a proactive and vigilant approach. Clinicians must maintain a high index of suspicion, particularly in patients from TB-endemic regions or those with a history of TB exposure. Relying solely on clinical symptoms or standard chest radiographs may prove insufficient. More sensitive diagnostic tools, such as sputum cultures, PCR-based assays, and interferon-gamma release assays (IGRAs), should be employed liberally, especially when there is any clinical ambiguity. Repeated testing may be warranted if initial results are negative but suspicion remains high.
Impact on Current Guidelines
Current guidelines from the American Thoracic Society (ATS) and the Centers for Disease Control and Prevention (CDC) recommend TB screening in high-risk individuals, including those with immunosuppression. However, these guidelines may not adequately address the unique challenges posed by SSc-associated ILD. The overlap in symptoms and the potential for atypical presentations warrant a more tailored approach. This is not to say the ATS or CDC guidance is wrong, simply that it was not designed with this specific patient population in mind. The 2019 EULAR recommendations for the management of systemic sclerosis do mention screening for latent TB before initiating immunosuppressive therapy, but they do not specifically address the nuances of patients already on immunosuppression who develop new pulmonary symptoms. Do we need to add further clarification for high TB burden areas?
Consider the 2021 ACR guidelines for rheumatoid arthritis: these detail recommendations on screening for latent TB before initiating biologic therapies. However, guidance for managing TB risk in SSc patients already on immunosuppressants, who then present with respiratory symptoms, remains less clear. A recent meta-analysis suggested that TNF inhibitors increase the risk of TB, but the risk with other immunosuppressants used in SSc (e.g., mycophenolate mofetil, cyclophosphamide) is less well-defined. More robust data are needed to guide risk stratification and screening intervals in this specific population.
Study Limitations
It is crucial to acknowledge the limitations inherent in case reports. While they can be valuable for highlighting unusual presentations and generating hypotheses, they cannot establish causality or provide definitive evidence to guide clinical practice. This particular case report describes a single patient, limiting the generalizability of the findings. Furthermore, the diagnosis of TB can be challenging, and there is always the possibility of misdiagnosis or delayed diagnosis, which could influence the interpretation of the case. The study also did not explore latent tuberculosis infection. Latent TB can reactivate with immunosuppression.
Moreover, the report does not delve into the specifics of the patient's immunosuppressive regimen, which could have influenced the risk of TB infection. The type and dosage of immunosuppressants, as well as the duration of treatment, are important factors to consider. Finally, it is important to note that the case report comes from a high TB burden country, which may limit its applicability to regions with lower TB prevalence. We need larger, prospective studies to assess the true incidence of TB in SSc patients and to identify specific risk factors.
Financial and Workflow Considerations
Implementing more aggressive TB screening strategies in SSc patients will inevitably have financial and workflow implications. The cost of IGRAs, sputum cultures, and PCR-based assays can be substantial, particularly if repeated testing is required. Furthermore, the interpretation of these tests can be complex, requiring expertise in both rheumatology and infectious disease. How do we ensure that patients have access to these tests, regardless of their insurance status or socioeconomic background? And how do we integrate these screening protocols into already overburdened clinical workflows?
Consider the workflow bottlenecks. If a patient screens positive for TB, they will require further evaluation and treatment, potentially involving multiple specialists and prolonged follow-up. This can strain already limited resources and create delays in care. Furthermore, the need for TB treatment may necessitate adjustments to the patient's immunosuppressive regimen, which can have implications for their SSc management. Clear protocols and interdisciplinary collaboration are essential to streamline the diagnostic and treatment process.
The financial toxicity associated with frequent TB screening, particularly in the context of ongoing immunosuppression, can be a significant barrier for patients. Many IGRAs are not universally covered by insurance, leaving patients with substantial out-of-pocket expenses. Moreover, the need for frequent monitoring and potential treatment adjustments can lead to increased healthcare utilization and associated costs. The workflow implications for rheumatology clinics are also considerable. Implementing routine TB screening requires dedicated staff time for test ordering, result tracking, and patient education. This can strain already limited resources and potentially delay care for other patients.
Reimbursement codes for TB screening in immunosuppressed individuals may not adequately reflect the complexity of these cases, potentially undercompensating providers for the time and resources required. Clearer guidelines and more appropriate reimbursement models are needed to ensure that clinicians are adequately supported in providing comprehensive care to SSc patients at risk for TB.
LSF-6195285834 | December 2025

How to cite this article
MacReady R. Systemic sclerosis and pulmonary tuberculosis risk. The Life Science Feed. Published December 24, 2025. Updated December 24, 2025. Accessed January 31, 2026. .
Copyright and license
© 2026 The Life Science Feed. All rights reserved. Unless otherwise indicated, all content is the property of The Life Science Feed and may not be reproduced, distributed, or transmitted in any form or by any means without prior written permission.
Fact-Checking & AI Transparency
This summary was generated using advanced AI technology and reviewed by our editorial team for accuracy and clinical relevance.
References
- Walker, U. A., Tyndall, A., Czirják, L., Denton, C., Khanna, D., Matucci-Cerinic, M., ... & Kowal-Bielecka, O. (2017). Clinical risk factors for digital ulcers in systemic sclerosis: a prospective study of EUSTAR centres. Annals of the rheumatic diseases, 76(1), 75-82.
- Kowal-Bielecka, O., Fransen, J., Avouac, J., Bérezné, A., Grindulis, K., de Groote, P., ... & Distler, O. (2017). Update of EULAR recommendations for the treatment of systemic sclerosis. Annals of the rheumatic diseases, 76(7), 1245-1258.
- Richmond, G. S., Hirani, A., Fernando, M. M., & Hayee, B. (2021). Tuberculosis risk with tumour necrosis factor alpha inhibitors and non-tumour necrosis factor alpha inhibitor biologics: a systematic review and meta-analysis. Alimentary pharmacology & therapeutics, 53(12), 1294-1305.