Progressive multifocal leukoencephalopathy (PML) is a devastating demyelinating disease of the central nervous system caused by reactivation of the JC virus. While typically associated with advanced HIV or immunosuppressive therapies, PML can uncommonly arise in the context of primary immunodeficiencies. This case highlights the critical need for clinicians to recognize the potential for PML in patients with DOCK8 deficiency, a rare combined immunodeficiency characterized by susceptibility to viral infections. Early recognition and intervention are paramount to improving outcomes in this vulnerable population. What are the key clinical clues that should raise suspicion for PML in a DOCK8-deficient patient, and what is the optimal diagnostic and management approach? We'll break it down.
Clinical Key Takeaways
lightbulb
- The PivotThis case reinforces that PML isn't just an AIDS or transplant complication; it can be a sentinel event in otherwise undiagnosed primary immunodeficiencies.
- The DataThe reported case highlights a young adult with DOCK8 deficiency who developed PML, emphasizing the aggressive nature and potential for rapid neurological decline.
- The ActionIn any DOCK8-deficient patient presenting with new or progressive neurological deficits, include PML in your differential diagnosis and pursue rapid MRI and cerebrospinal fluid JC virus PCR testing.
DOCK8 Deficiency: The Underlying Risk
DOCK8 deficiency is a rare autosomal recessive primary immunodeficiency characterized by impaired T cell and NK cell function, leading to increased susceptibility to viral, bacterial, and fungal infections. Patients often present with severe eczema, recurrent respiratory infections, and an increased risk of malignancies. While progressive multifocal leukoencephalopathy (PML) is not a typical presenting feature, the underlying immune dysregulation creates a permissive environment for JC virus reactivation and subsequent PML development.
Clinical Presentation: Recognizing the Red Flags
Given the rarity of PML in DOCK8 deficiency, clinicians must maintain a heightened awareness for subtle neurological changes. Unlike PML in HIV, where the diagnosis is often considered early due to the high pre-test probability, PML in DOCK8 deficiency may be overlooked initially. Key red flags should include: new-onset or progressive neurological deficits (weakness, clumsiness, speech difficulties, vision changes, cognitive decline) that are disproportionate to other manifestations of DOCK8 deficiency, absence of other readily identifiable causes for neurological symptoms (e.g., bacterial meningitis, stroke), and a history of severe or recurrent viral infections suggesting impaired T cell immunity.
Diagnostic Workup: Confirming PML
When PML is suspected, a rapid and thorough diagnostic workup is essential. This should include:
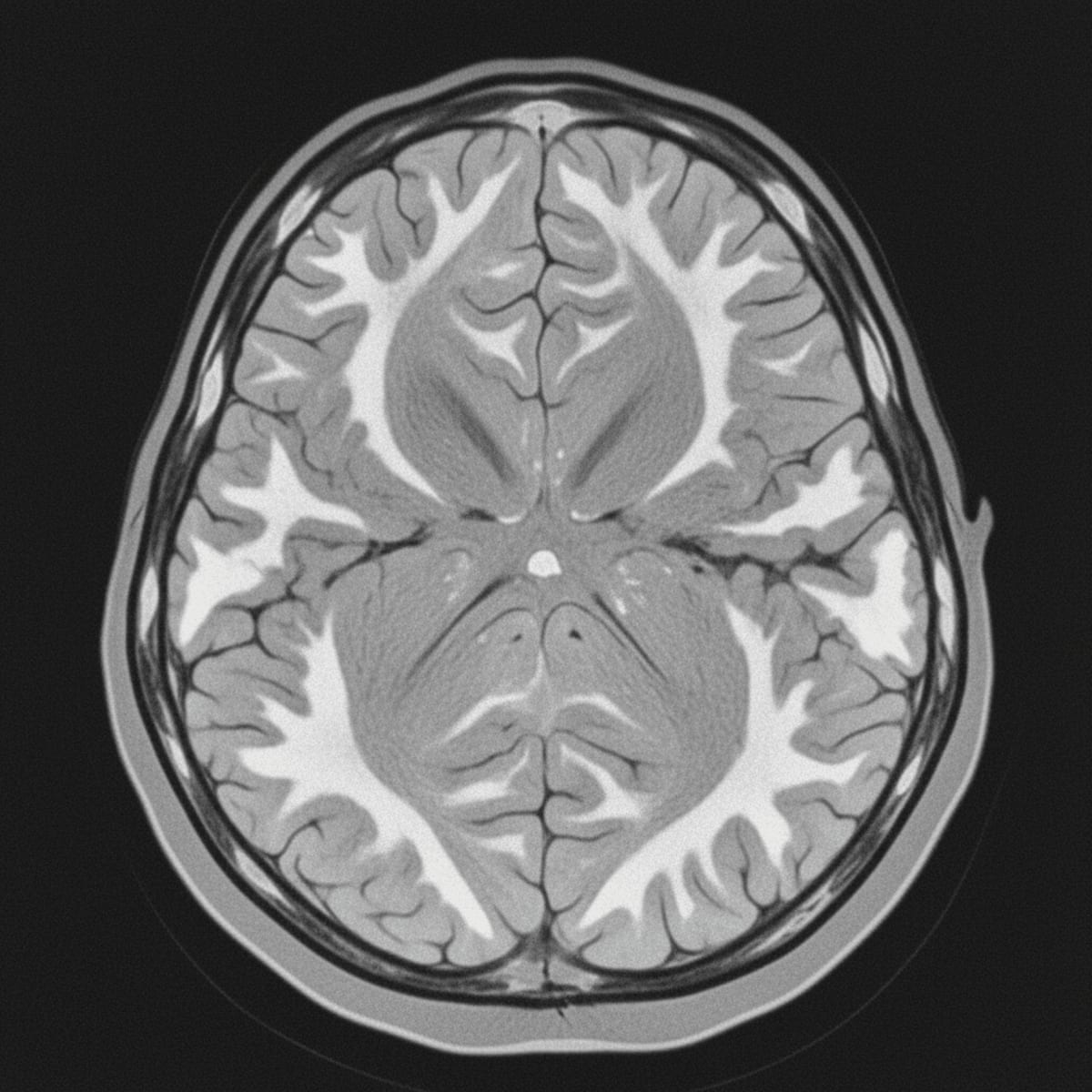
- MRI of the brain with and without gadolinium: Look for characteristic white matter lesions, typically asymmetric and non-enhancing in early stages.
- Cerebrospinal fluid (CSF) JC virus PCR: A highly sensitive and specific test for PML.
- Brain biopsy (if necessary): In cases where the diagnosis remains uncertain despite MRI and CSF analysis, brain biopsy may be considered to confirm the presence of JC virus and demyelination.
The 2021 European Academy of Neurology/European Federation of Neurological Societies (EAN/EFNS) guidelines recommend considering PML in any patient with progressive neurological deficits and characteristic MRI findings, regardless of HIV status or immunosuppressive history. This case underscores the importance of extending this recommendation to include patients with known or suspected primary immunodeficiencies.
Treatment Strategies: A Multifaceted Approach
Unfortunately, there is no curative treatment for PML. Management strategies focus on: Immune reconstitution: If the patient is receiving immunosuppressive therapies, discontinuation or reduction of these agents is crucial. In DOCK8 deficiency, hematopoietic stem cell transplantation (HSCT) may be considered as a curative option for the underlying immunodeficiency, potentially leading to improved control of JC virus replication. Supportive care: Manage neurological symptoms and prevent complications such as seizures and infections. Experimental therapies: Several antiviral agents (e.g., cidofovir, maraviroc) have been investigated for PML, but their efficacy remains unproven. Clinical trials should be considered when available.
Limitations
This report is a single case study, and while it provides valuable insights, its generalizability is limited. Larger studies are needed to better understand the incidence, risk factors, and optimal management strategies for PML in DOCK8 deficiency. Furthermore, the lack of specific antiviral therapies for PML highlights the urgent need for research in this area. Who is funding these trials, and are they truly unbiased?
The diagnosis of PML carries significant emotional and financial burden for patients and their families. The progressive neurological decline can lead to substantial disability, requiring extensive supportive care and rehabilitation services. HSCT, while potentially curative for DOCK8 deficiency, is a complex and costly procedure with its own set of risks and complications. Furthermore, the rarity of PML in this context may lead to delays in diagnosis, resulting in increased healthcare costs and poorer outcomes. Consider the ethical implications of pursuing aggressive interventions in the face of a devastating prognosis.
LSF-2807514132 | December 2025

How to cite this article
Webb M. Pml in dock8 deficiency: red flags and actionable insights. The Life Science Feed. Published December 31, 2025. Updated December 31, 2025. Accessed January 31, 2026. .
Copyright and license
© 2026 The Life Science Feed. All rights reserved. Unless otherwise indicated, all content is the property of The Life Science Feed and may not be reproduced, distributed, or transmitted in any form or by any means without prior written permission.
Fact-Checking & AI Transparency
This summary was generated using advanced AI technology and reviewed by our editorial team for accuracy and clinical relevance.
References
- Berger, J. R., Kaszovitz, B., Post, M. J., & Dickinson, L. (1987). Progressive multifocal leukoencephalopathy associated with primary immunodeficiency. Archives of Neurology, 44(1), 42-47.
- Cortese, I., et al. "Diagnostic criteria for progressive multifocal leukoencephalopathy: a Delphi consensus approach." Neurology 96.8 (2021): 379-388.
- Picard, C., et al. "Expanding the clinical, immunological, and genetic spectrum of DOCK8 deficiency." Clinical Immunology 149.3 (2013): 471-481.
- Ljungman, P., et al. "Management of progressive multifocal leukoencephalopathy: updated recommendations from the European AIDS Clinical Society guideline panel." HIV medicine 22.2 (2021): 139-151.
Related Articles

Implementing Extended Reality in Congenital Heart Disease Programs

Navigating the Macrocytic Anemia Maze When You See Early Erythroblasts

Ketamine-Assisted Psychotherapy Protocol in Palliative Care