Polycystic ovary syndrome (PCOS) is not just a reproductive disorder; it’s a metabolic and psychological challenge with significant implications for long-term health and healthcare spending. When patients fail to adhere to recommended lifestyle modifications or medication regimens, the consequences reverberate across the healthcare system, driving up costs associated with downstream complications. These complications include infertility treatments, management of type 2 diabetes, cardiovascular disease, and even increased risk for certain cancers.
The question isn’t simply about individual patient responsibility. It’s about how we, as a healthcare community, can create systems that support sustained adherence and mitigate the economic fallout of poorly managed PCOS. What are the hidden costs, and who ultimately pays the price?
Clinical Key Takeaways
lightbulb
- The PivotPCOS non-adherence should be viewed as a systemic issue requiring multifaceted interventions, not just a failure of individual patient behavior.
- The DataPoorly managed PCOS increases the risk of type 2 diabetes by up to 4-fold, dramatically raising long-term healthcare expenditure.
- The ActionAdvocate for policy changes that improve access to multidisciplinary care teams (endocrinologists, dietitians, psychologists) and address the financial burden of PCOS management for patients.
Guideline Discordance and Costs
Current guidelines from the American College of Obstetricians and Gynecologists (ACOG) and the Endocrine Society emphasize lifestyle modifications, such as diet and exercise, as first-line treatments for PCOS. However, a significant disconnect exists between these recommendations and actual patient adherence. This non-compliance directly translates into increased healthcare utilization and costs. For instance, patients who do not adhere to lifestyle changes or prescribed medications (like metformin or oral contraceptives) are more likely to require expensive interventions such as fertility treatments (IVF, ovulation induction) or long-term management of type 2 diabetes and cardiovascular complications. These costs are often borne by insurers and, ultimately, passed on to consumers through higher premiums.
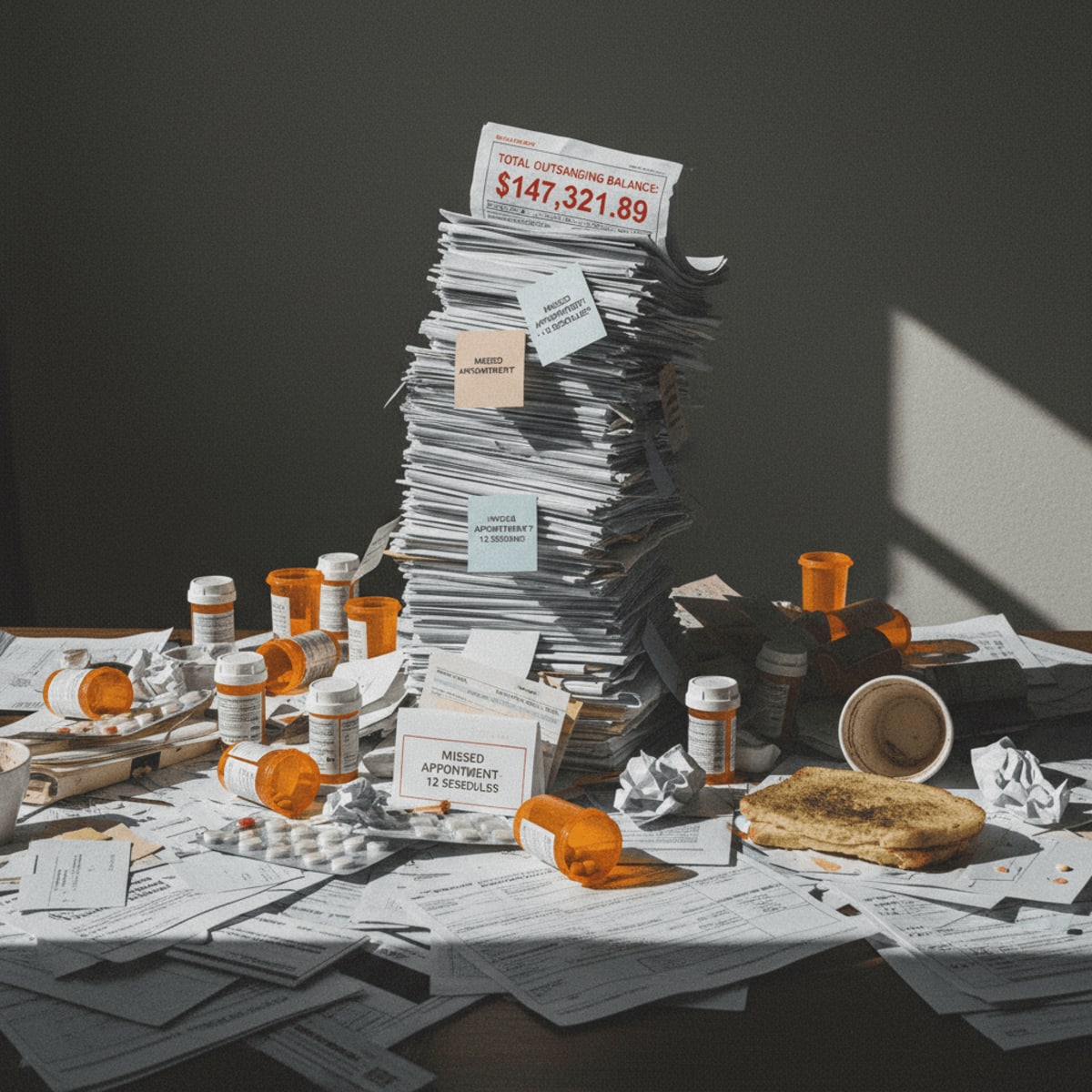
Consider the cost of infertility treatment: a single IVF cycle can cost upwards of $15,000, and many patients require multiple cycles. Now factor in the increased risk of gestational diabetes, pre-eclampsia, and cesarean sections associated with pregnancies achieved through assisted reproductive technologies. These downstream costs accumulate rapidly, placing a strain on both individual families and the healthcare system as a whole.
The Challenge of Adherence
Adherence isn't solely a matter of patient willpower. Socioeconomic factors, access to care, and cultural beliefs all play a significant role. Many women with PCOS lack access to specialized endocrinologists or registered dietitians who can provide personalized guidance on diet and exercise. Furthermore, the financial burden of PCOS management, including the cost of medications, supplements, and regular doctor's visits, can be prohibitive for low-income individuals. We need to address these systemic barriers to improve adherence rates.
The psychological impact of PCOS also contributes to non-compliance. Symptoms like hirsutism, acne, and weight gain can lead to depression, anxiety, and body image issues, making it even more challenging for women to stick to healthy lifestyle habits. These mental health challenges often go unaddressed, further exacerbating the problem. A more holistic approach that integrates mental health support into PCOS care is essential. The absence of that translates directly into dollars spent managing downstream, preventable disease.
Study Limitations and Real-World Considerations
Any analysis of PCOS adherence is limited by the heterogeneity of the syndrome itself. PCOS presents differently in different individuals, with varying degrees of hormonal imbalances, metabolic dysfunction, and reproductive issues. This makes it difficult to develop one-size-fits-all interventions that are effective for everyone. Moreover, most studies on PCOS adherence are retrospective, relying on self-reported data or medical records, which may be incomplete or inaccurate. The reliance on observational data introduces the risk of confounding variables that are difficult to control for.
It is also critical to acknowledge that the long-term effectiveness of PCOS treatments is not always well-established. While medications like metformin and oral contraceptives can help manage symptoms, they do not address the underlying causes of the syndrome. This can lead to frustration and disillusionment among patients, further contributing to non-adherence. The lack of a definitive cure for PCOS underscores the need for ongoing research into novel therapeutic targets and strategies.
Workflow integration
Integrating adherence support into existing clinical workflows is crucial. This could involve training primary care physicians to screen for PCOS and provide basic lifestyle counseling, or establishing dedicated PCOS clinics staffed by multidisciplinary teams. Telehealth solutions can also play a role in improving access to care, particularly for women living in rural areas or those with limited mobility.
Payers also have a role to play. Incentivizing adherence through reduced co-pays for medications or offering financial assistance for lifestyle programs can help make PCOS management more affordable and accessible. Furthermore, payers should consider reimbursing for comprehensive PCOS care that includes mental health support and nutritional counseling. A shift towards value-based care models that reward outcomes rather than volume could also incentivize providers to prioritize adherence and long-term patient well-being. The long-term savings far outweigh the initial investment. Let's not let short-sighted budget concerns dictate substandard care for this significant patient population.
The economic consequences of PCOS non-adherence extend beyond direct medical costs. Lost productivity due to illness, disability, and premature mortality also contribute to the overall economic burden. Furthermore, the psychological distress associated with PCOS can impact women's quality of life and their ability to participate fully in society.
From a policy perspective, there is a clear need for greater investment in PCOS research, prevention, and management. This includes funding for studies to identify the underlying causes of PCOS, develop more effective treatments, and evaluate the impact of different adherence interventions. It also requires raising awareness about PCOS among healthcare professionals and the general public, reducing stigma, and empowering women to take control of their health.
There's also a need to address potential workflow bottlenecks. If we emphasize increased dietician visits for these patients, are those dieticians available? Will insurance reimburse these visits? These are the questions that must be answered to drive true improvements in PCOS management.
LSF-0934395728 | December 2025

How to cite this article
Gellar S. The systemic price of pcos non-adherence. The Life Science Feed. Published December 15, 2025. Updated December 15, 2025. Accessed January 31, 2026. .
Copyright and license
© 2026 The Life Science Feed. All rights reserved. Unless otherwise indicated, all content is the property of The Life Science Feed and may not be reproduced, distributed, or transmitted in any form or by any means without prior written permission.
Fact-Checking & AI Transparency
This summary was generated using advanced AI technology and reviewed by our editorial team for accuracy and clinical relevance.
References
- Azziz, R., Carmina, E., Chen, Z., Dunaif, A., Laven, J. S., Legro, R. S., ... & International PCOS Network. (2016). Polycystic ovary syndrome: criteria for diagnosis and definition. Fertility and Sterility, 106(1), 13-21.
- Teede, H. J., Misso, M. L., Costello, M. F., Dokras, A., Laven, J., Moran, L., ... & International PCOS Network. (2018). Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Human Reproduction, 33(9), 1602-1618.
- Goodman, N. F., Cobin, R. H., Futterweit, W., Glueck, J. S., Legro, R. S., Carmina, E., & American Association of Clinical Endocrinologists. (2015). American Association of Clinical Endocrinologists, American College of Endocrinology, and Androgen Excess and PCOS Society disease state clinical review: guide to the best practices in the evaluation and treatment of polycystic ovary syndrome-part 1. Endocrine Practice, 21(11), 1291-1300.
Related Articles



The Business Case for Multidisciplinary Limb Programs in Peripheral Arterial Disease